Ultrasound in pregnancy
Fetal ultrasound scans
At our centre we offer comprehensive ultrasound diagnostics in pregnancy. The examination aims to assure parents that the fetus develops normally.
After diagnosing abnormality, we always feel obliged to take special care of parents. In difficult moments, we put much effort to limit appointments to the essential minimum. We present the diagnosis during the first visit, and provide detailed information in a simple and clear way. Close cooperation with paediatricians gives us an opportunity to provide you with a consultation, even during pregnancy if necessary. We are here for you, and our support is supposed to bring parents maximum comfort.
We offer ultrasound examinations in each trimester and week of gestation. For a fetus which develops normally, the optimal schedule, advised by specialists, is presented in the table below:
| I trimester | II trimester | III trimester | |
|---|---|---|---|
| Weeks | 11+0 – 13+6 Optimally 12+ |
18 – 20 | 28 – 32 |
In each questionable case, the ultrasound scan is performed immediately. It is important to mention the problem during registration. Our receptionist will set a date and time convenient for you.
Early pregnancy and reproductive organ assessment up to 10 weeks
The aim of this scan is the confirmation of pregnancy, assessing its localization, development and carrying out detailed measurements of a gestational sac (GS), embryo (Crown Rump Length – CRL) and yolk sac (YS). We also measure fetal heart rate (FHR). In case of a multiple pregnancy, this is the stage when we assess the number of placentas and amniotic sacs, which has a great importance for further diagnosis and proceeding in the course of pregnancy.
Additionally, we assess the structure of uterus and ovaries. We also extend the range of measurements individually if necessary.




11+0 to 13+6 weeks late first trimester scan. Chromosomal aberrations risk assessment with an early fetal cardiac and extracardiac assessment.
It is the most important scan during pregnancy. This examination should be preferably carried out in 12 weeks + several days of gestation.
A fetus, though still small, has developed majority of organs. A correctly performed ultrasound scan (an early fetal anatomy scan) allows to exclude over half of congenital defects and calm parents already at this stage.
Why is it so early? Since the majority of congenital defects arise at an early stage of pregnancy, there is no reason to postpone the diagnosis. Some of congenital defects are even more visible, and therefore easier to diagnose, in early pregnancy.
An early fetal anatomy scan includes the assessment of: skull, brain chest with the heart, abdominal cavity and walls, diaphragm, stomach, kidneys, bladder, skeleton, i.e. chest and limbs. It is also essential to assess two fetal biometric parameters: crown rump length (CRL) which is used to calculate the gestational age and expected delivery time, as well as the biparietal diameter of the fetal head.
An early fetal echocardiography allows to assess the arrangement of viscera (stomach, liver, heart), heart position and its axis, inflow into both cavities and position of large blood vessels, interventricular septum and “cardiac crux”.
In multiple pregnancies it is essential to estimate the number of placentas and amniotic sacs. An examination in the 12th week of gestation is the last optimal chance to acquire such information. It is of a great importance in further diagnosis and medical care during this kind of pregnancy.




Another, very important aim of examination at 12 weeks of gestation is to assess the ultrasound parameters, so called markers, which are used to assess the fetal genetic risk for a given pregnancy. Genetic disorders constitute a large group of neonatal complications and their detection is the most effective at this stage of pregnancy. The assessment of genetic markers is not an obligatory part of examination, it can be omitted at parents’ request, then the scan involves only a detailed anatomical assessment.
Parameters, which can influence the risk of most common genetic syndromes are listed in the table below.
| Ultrasound parameters Markers | Congenital defects | Soft ultrasound markers | Biomarkers | Background risk |
|---|---|---|---|---|
| nuchal translucency | holoprosencephaly | Choroid plexus cysts | free β-HCG level in serum of a pregnant woman | Maternal age |
| fetal heart rate | Diaphragmatic hernia | Hyperechogenic bowels | PAPP-A hormone level in serum of a pregnant woman | family history indicating the higher risk of genetic syndromes |
| ossification of the nasal bone | Omphalocele | renal pelvis dilatation | ||
| ductus venosus flow assessment | Atrioventricular septal defect | Echogenic intracardiac focus | ||
| tricuspid valve flow | Megacystis |




We are the only cenrte in Krakow and Lesser Poland, which uses complete computer algorithms to calculate the risk of chromosomal aberrations, according to the Fetal Medicine Foundation guidelines. It helps to achieve a a high test accuracy which exceeds 90%. We have a vast experience in diagnosing disorders, such as the Down syndrome. We carefully analyze our patients’ test results, which allow us to consult patients basing on our own cases and experience. Our attitude is what distinguishes us from other diagnostic centres.
What does it look like and how to interpret the results? The test results in 12 weeks of gestation are presented as the individual risk estimated for a given pregnancy. The result shows whether the examination provides enough information about the patient and if the most common genetic disorders are possible to exclude. A great majority of results are satisfying. An increased risk (greater than or equal to 1:100) is found in a small percentage of cases. However, it does not mean that the baby is sick! It is important to acknowledge that the screening test is not sufficient and it is essential to conduct additional tests (see: amniocentesis/ chorionic villus sampling sections)
In some cases during the 11+0 – 13+6 test, it is recommended to assess the risk of preeclampsia, connected with hypertension (involving 2% of pregnancies) as well as the risk of Intrauterine Growth Restriction (IUGR). This complication may involve even 5% of pregnancies. The assessment is based on parameters of blood flow in uterus arteries and the history, including the height and weight of a pregnant woman.




16-20 weeks: Genetic and anatomical examination „genetic ultrasound”
It is a particularly recommended element of the 2nd trimester examination for patients, who have not undergone screening tests in the first trimester. It is also recommended to women whose result of 12 weeks examination indicated an increased genetic risk, however, they refused to undergo conclusive tests.
Genetic ultrasound combines anomaly scan, i.e. fetal anatomic examination as well as the ultrasound parameters assessment, which constitute a group of second trimester genetic markers. As during first trimester scan, genetic ultrasound aims to calm parents and convince them that the risk of genetic disorders, such us the Down syndrome, is low.
Makers are specific features of fetal “beauty” that are more common among children with genetic syndromes, although, as an isolated feature, they can also occur in healthy individuals. Compilation of markers, i.e. the occurrence of several features in one fetus, significantly increases the genetic risk and obliges the specialist to recommend additional tests such as amniocentesis or fetal blood sampling.
Genetic ultrasound is a method developed in the United States and based on women between 16 and 20 weeks of gestation. It is essential to stick to the same time frame, the test should not be carried out after 20 weeks since then the test accuracy is significantly reduced.
The result of the examination may be presented as an estimated risk – a numerical value – a fraction. The assessment of second trimester „genetic” risk is conducted with the use of transabdominal transducer in most cases. However, in certain situations, transvaginal scan is required.




Down Syndrome Soft Ultrasound Markers:
- Thickened Nuchal Fold,
- delay in forming nasal bones (NB- ang. Nasal Bone),
- Increased Prenasal Thickness,
- a short femur or humerus length,
- flat facial profile and an increased frontomaxillary facial angle,
- enlarged lateral ventricles in the brain,
- hyperechogenic bowels,,
- significant fetal tricuspid regurgitation,
- Pericardial Effusion,
- ventricular disproportion in the fetal heart,
- incorrect atrioventricular valve attachment,
- glossomegaly,
- hypertelorism,
- interspace between the great toe of the foot from the rest of the toes (sandal gap),
- short middle phalanx of the 5th finger,
- Aberrant Right Subclavian Artery,
- wide iliac angle.
Congenital defects coexisting with the Down syndrome:
- cardiac defects, most most frequently atrioventricular septal defect type A (1000 times more often than in healthy babies)
- digestive tract defects such as duodenal atresia, small intestine obstruction, esophageal atresia, Hirschsprung’s disease (67 times more often),
- microcephaly (12 times more often),
- facial defects (9 times more often),
- hydrocephaly (8 times more often),
- abdominal walls defects (6.5 times more often),
- diaphragmatic hernia (6 times more often),
- urinary tract anomalies (3.5 times more often).
During this scan we usually measure: fetal heart rate; biometric parameters, including the measurement of the head, abdomen, femur and humerus; transverse cerebellar diameter; nuchal fold thickness; nasal bone length; prenasal thickness; fronto-maxillary angle; blood flow in ductus venosus.
If necessary, the measurement protocol can be adjusted to individual needs.




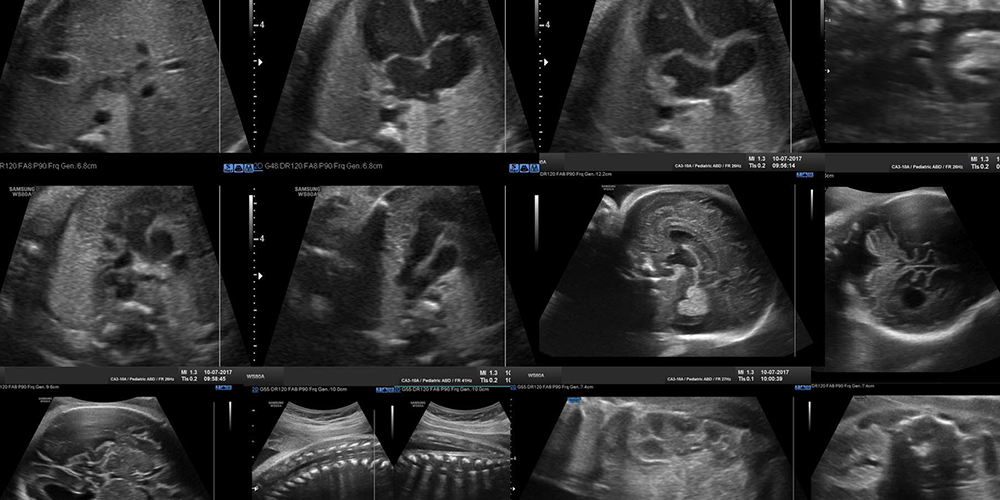
18 – 23 weeks: anomaly scan with included a detailed cardiac scan
This scan consists in an assessment of a fetal development and anomaly scan. It complements the late first trimester scan and it allows to analyze fetal anatomy and exclude a significant group of congenital defects.
Anatomical examination involves an assessment of: head (eyes, mouth, nose, ears); skull (calcification, bone formation, including hard palate), neck, chest (ribs, lungs, heart, diaphragm, thymus); abdominal cavity (abdominal walls, liver, gallbladder, stomach, kidneys, intestines), minor pelvis (bladder, rectum, iliac wings, umbilical arteries), vertebral column (calcification, curves, vertebral arches and bodies structure, covering tissues), limbs (anatomical structure and joints mobility).
Additionally, we assess uterine structure, amount of amniotic fluid and placenta. In case of twin pregnancies the scan protocol includes peripheral vascular flow aassessment as well.
In an anomaly scan we include detailed cardiac assessment on the basis of fetal echocardiography guidelines published by ISUOG in 2023.
In case of diagnosing anomalies, a specialist is obliged to recommend extended diagnosis.
We usually measure: the fetal heart rate; biometric parameters including the measurements of the head, abdomen, femur and humerus; transverse cerebellar diameter; nuchal fold thickness; nasal bone length; ductus venosus blood flow; the length of a cervical canal.
If necessary, the measurement protocol can be adjusted to individual needs.




28 – 32 weeks: Fetal growth and well-being scan
Ultrasound scan in the third trimester is a very important stage of fetal examination. The aim of this scan is an assessment of a fetal development, its well-being and anatomy. Although the probability of anomalies (if two previous examinations did not indicate any abnormalities) is low, it is essential to exclude defects, which might occur later in the course of pregnancy.
Biometric parameters assessment in the third trimester allows to estimate fetal growth parameters and weight gain. Blood circulation and well-being are normally assessed basing on three vessels: umbilical artery, middle cerebral artery and ductus venosus. Among congenital defects, which occur later, there are: microcephaly, cerebellar hypoplasia, duodenal atresia and other intestines defects, some of the uterine system defects, some of the limbs defects, ventricular septal defects and dynamical heart defects, including pulmonary valve stenosis, aortic coarctation, anomalies of atrioventricular valves, e.g. dysplasia. Previously mentioned pulmonary valve stenosis, according to American research, is the second common heart defect and at the same time, one of the rarest anomalies detected in fetal life. Some small ventricular septal defects are not visible before the third trimester, therefore, this scan allows to diagnose this disorder.
We usually measure: the fetal heart rate; biometric parameters, including the head, abdomen, femur, transverse cerebellar diameter; blood flow in umbilical artery, middle cerebral artery and ductus venosus; intracardiac blood circulation; amniotic fluid index.
If necessary, the measurement protocol can be adjusted to individual needs.





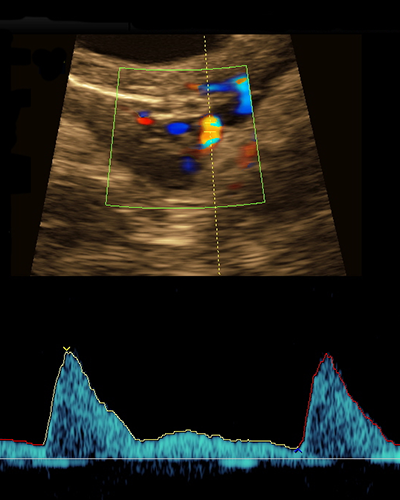
Fetal cardiac scan
The most important element of a fetal anatomy assessment is the cardiac evaluation. We perform fetal cardiac examinations according to the sequential, segmental analysis, which is in line with the postnatal evaluation. We follow recommendations of the International Society of Ultrasound in Obstetrics and Gynecology (2023) and American Society of Echocardiography (2023). In each case, the examination protocol includes an assessment of: cardiac axis and visceral arrangement, cardiac chambers morphology, veno-atrial, atrio-ventricular, ventriculo-arterial connections; aortic arch and arterial duct; interventricular septum; interatrial septum and foramen ovale.
Normally, during fetal cardiac examination in the third trimester and in each case of suspected stenosis we conduct the spectral Doppler velocimetry.
Fetal heart defects constitute over 1/3 of all congenital disorders, and we are experienced in their detection. We start the diagnosis in the first trimester at 12 weeks of gestation, since it is the time when we can exclude the majority of the most serious anomalies.
We work in cooperation with an experienced cardiac surgeon, who if necessary, can provide specialist consultations already during pregnancy, basing on our scan findings.
Any fetal cardiac scan indicating a cardiac defect in the course of pregnancy is not fully conclusive. All the decisions concerning a surgery are taken on the basis of an echocardiographic scan performed after delivery.
Congenital Heart Disease may be connected with genetic syndromes, therefore, in those particular cases we recommend chromosome abnormalities test of a baby (genetic assessment by means of amniocentesis or fetal blood sampling).
We usually measure: velocities and blood flow parameters in an ascending aorta, pulmonary artery, ductus arteriosus, through tricuspid valve, mitral valve, in ductus venosus and pulmonary veins; cardiac chamber sizes and large vessels width represented in a form of standard deviations toward head and femur measurements (Z-scores); fetal heart rhythm, atrio-ventricular conduction time.








Additional check-up examinations
Among some patients, e.g. in cases of twin pregnancies or detected anomalies, it is necessary to carry out ultrasound check-up scans.